What is cerebrospinal fluid?
CSF leakage is a pathological condition in which cerebrospinal fluid (CSF) leaks from natural openings or injuries in the meninges. It can occur due to trauma, surgery, or for no apparent reason. CSF leakage can be a serious threat to the patient’s health, as it opens the way for infection to enter the brain and can lead to meningitis or other complications.
A rupture of the dura mater covering the base of the skull can occur with:
- Skull fractures
- Inflammatory diseases of the meninges and bones of the sinuses.
- Congenital developmental anomalies.
The main causes of cerebrospinal fluid:
- Traumatic – occurs due to damage to the skull or spine due to injuries.
- Postoperative – occurs after surgical interventions, in particular operations on the brain, skull base, or sinuses.
- Spontaneous – occurs without apparent cause and is associated with defects in the meninges.
Types of cerebrospinal fluid
- nasal cerebrospinal fluid (CSF leakage from the nose),
- otosyringorrhea (leakage of cerebrospinal fluid from the ear),
- cerebrospinal fluid from postoperative wounds, after craniotomy,
- wounds in compression fractures.
The very presence of cerebrospinal fluid indicates direct communication of the subarachnoid space of the cranial cavity with the external environment with the threat of infection and the development of purulent-inflammatory complications:
- meningitis,
- brain abscesses,
- encephalitis.
Symptoms of cerebrospinal fluid:
- Clear or yellowish discharge from the nose or ears.
- Headaches that decrease in a horizontal position.
- Tinnitus, dizziness.
- Increased fatigue.
Diagnostics:
- Laboratory tests to determine cerebrospinal fluid in secretions (β2-transferrin test).
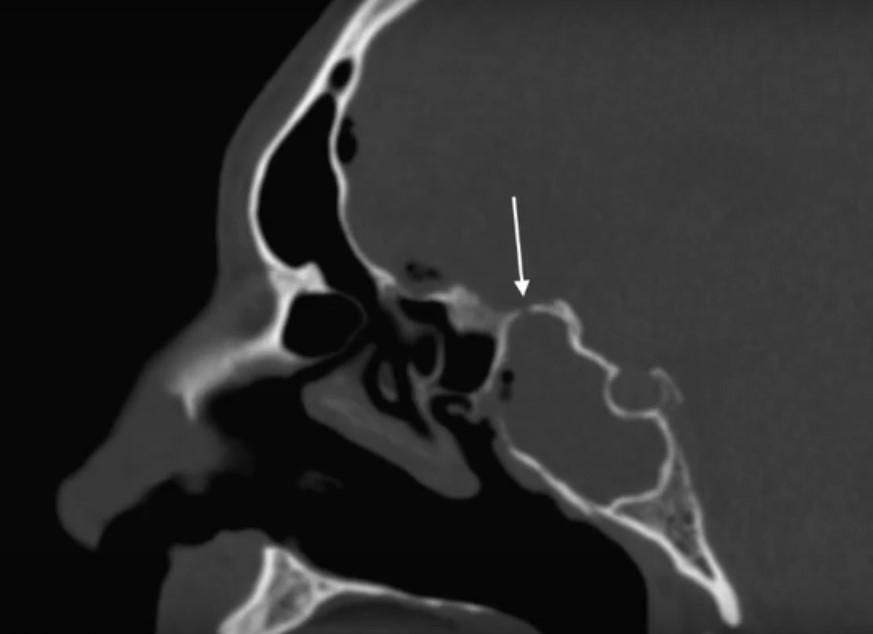
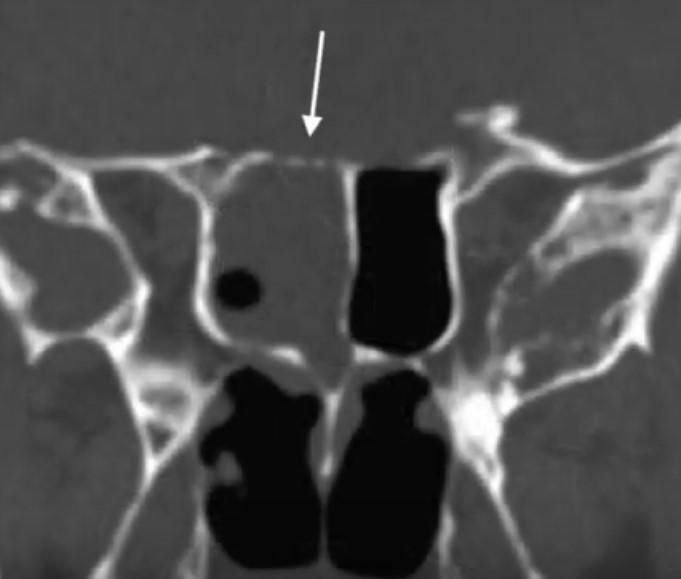
- CT and MRI to identify the location of the leak.
- Endoscopic examination of the nasal cavity and skull.
CSF leakage is the leakage of cerebrospinal fluid (CSF) from the brain due to injury or other disease. Normally, cerebrospinal fluid (CSF) “washes” the brain and is the content of the ventricles of the brain. CSF is produced by the choroid plexuses of the brain and normally circulates from the ventricles into the subarachnoid space, where it is absorbed into the venous system through venous granulations.
In the case of the development of cerebrospinal fluid, a direct connection of the subarachnoid space with the external environment appears, which leads to serious infectious complications from the nervous system (meningitis, encephalitis, ventriculitis).
This process can occur as a result of trauma, surgery, or spontaneously. Diagnosis of cerebrospinal fluid is critically important because its untimely detection can lead to serious complications such as meningitis or chronic intracranial hypotension.
There are the following types of cerebrospinal fluid:
CSF leakage can be classified into several main types depending on the cause:
- Nasal cerebrospinal fluid (CSF) leakage from the nose.
- Oto-CSF leakage is the leakage of cerebrospinal fluid from the ear, postoperative CSF leakage is the leakage of cerebrospinal fluid from the wound after neurosurgical operations.
- Traumatic cerebrospinal fluid. Occurs as a result of mechanical damage to the head, which can be caused by trauma or surgery to the skull, face, mouth, or nose. Approximately 2% of patients who have suffered a serious head injury suffer from post-traumatic cerebrospinal fluid. In most cases (80%) such cerebrospinal fluid resolves spontaneously within the first week after the injury.
- Postoperative (iatrogenic) cerebrospinal fluid. Occurs as a result of surgical manipulations, most often on the skull or in the sinuses. The frequency of this type of cerebrospinal fluid reaches 16% among patients who have undergone operations in the craniobasal region, such as the removal of tumors. Postoperative cerebrospinal fluid is especially common after the removal of tumors in the area of the base of the skull.
- Spontaneous cerebrospinal fluid loss. This syndrome is idiopathic and differs from traumatic forms in that it has no apparent cause. It may be caused by natural defects in the dura mater. Rapid loss of cerebrospinal fluid results in intracranial hypotension, a condition characterized by decreased intracranial pressure.
In typical cases, the diagnosis of cerebrospinal fluid is not difficult; for differential diagnosis, an analysis of the leaking fluid is performed, which helps to establish the diagnosis. Head tilt tests, Stukey’s tests, and Queckenstedt’s tests, which enhance the discharge of cerebrospinal fluid, are helpful in detecting cerebrospinal fluid.
Clinical signs
The main clinical manifestations of cerebrospinal fluid leakage depend on the location of the leak and its intensity. The following symptoms are most often observed:
- Clear discharge from the nose or ears (with nasal or ear cerebrospinal fluid);
- Headaches, especially when standing (a sign of intracranial hypotension);
- Tinnitus, dizziness;
- Feeling of pressure in the eyes or face;
- Decreased hearing or sense of smell (if the corresponding anatomical structures are affected).
Patients may complain of a squeezing headache that worsens when standing, nausea, and thirst.
When signs of infection develop, the condition worsens, there is: an increase in body temperature to 39-40 degrees, depression of consciousness, meningeal symptoms, there may be convulsions. In difficult cases, as well as for the diagnosis of “hidden” cerebrospinal fluid, special tests are performed (spinal puncture with the introduction of dyes), endoscopic examination of the nose and ear.
They also perform brain cisternography, which involves injecting a contrast agent into the subarachnoid space through spinal puncture, followed by computed tomography in special setups.
Methods for diagnosing cerebrospinal fluid
Several key methods are used to diagnose cerebrospinal fluid (CSF) leakage, aimed at accurately identifying the location of the leak and assessing its volume.
- Clinical examination : One of the most important aspects of the evaluation is the history and physical examination of the patient. The physician should note the presence of clear nasal or ear discharge and other signs of intracranial hypotension.
- Laboratory tests . Laboratory analysis of secretions for the presence of the protein β2-transferrin is the most specific method for confirming cerebrospinal fluid, since this protein is present exclusively in cerebrospinal fluid.
- Visualization methods :
- CT (computed tomography) with contrast can identify anatomical defects and pinpoint the exact location of fluid leakage.
- MRI (magnetic resonance imaging) is an additional method for evaluating soft tissue and meningeal injuries.
- CT cisternography is used to assess the spread of contrast medium through the fistulous canal.
- Endoscopic examination . If nasal or ear cerebrospinal fluid is suspected, endoscopic examination can help identify the location of the membrane defect and determine the need for surgical correction.
Timely diagnosis of cerebrospinal fluid (CSF) leakage is critical to preventing serious complications. The use of modern imaging and laboratory techniques allows for accurate identification of the cause and location of the leak, which facilitates effective treatment and recovery of the patient.
Treatment
Treatment of cerebrospinal fluid (CSF) leakage should be initiated as soon as possible to seal the subarachnoid space. This can be achieved surgically or with the conservative treatments described below.
Treatment of cerebrospinal fluid (CSF) depends on the cause and severity of the leak. In most cases, conservative treatment, including bed rest, correction of intracranial pressure, and observation, is recommended. If the leak does not stop within 7–10 days, surgery may be required to close the fistula.
Rapid diagnosis and timely treatment of cerebrospinal fluid (CSF) are key to preventing complications and preserving the patient’s health.
Conservative treatment of cerebrospinal fluid
Liquorrhea can be both an independent disease and a complication of a traumatic brain injury or other diseases. In general, liquorrhea is the leakage of fluid that surrounds the brain and spinal cord to the outside through unnatural openings. Some of them are formed as a result of trauma, others are congenital or acquired as a result of tumor or inflammatory diseases, appear after operations on the skull and in the nasal cavity, on the bone apparatus of the ear.
Liquorrhea: the greatest danger of liquorrhea is the penetration of infection into the cranial cavity, therefore, if symptoms appear: abundant discharge of clear fluid from the nose or ear, accompanied by a headache, it is necessary to immediately consult a neurosurgeon and ENT doctor. At the first stage of treatment, conservative therapy is prescribed, if it is ineffective, the patient will be offered surgical intervention.
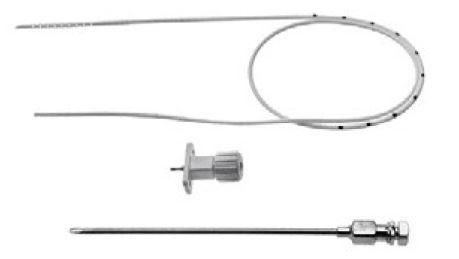
As a rule, lumbar drainage is first installed – the thinnest catheter, which will drain the cerebrospinal fluid, preventing it from pouring out of the cranial cavity, thus creating conditions for the pathological course to heal, usually the catheter is installed for 5-7 days. Also, it is mandatory to prescribe: antibiotic therapy to prevent infectious complications, diuretics are prescribed to reduce intracranial pressure, anti-inflammatory therapy. During treatment, the patient is recommended to keep the head elevated, avoid: coughing, abdominal tension and sniffing, mechanical cleaning of the ears.

If the patient continues to have nasal discharge during treatment or recovery after treatment, surgical intervention is recommended. If the described complaints appear, consult a doctor as soon as possible, remember, preventing possible complications is much easier than treating them. The neurosurgical department of the Kherson Regional Clinical Hospital has accumulated vast experience in treating liquorrhea.
Doctors Zhuravlev O.F., Leontiev O.Yu.
Neurosurgeons Malyshenko M.P. and Dmytruk V.S.
Стаття написана: 22.01.2026
Стаття перевірена медичним спеціалістом: 23.01.2026
Popular destinations:
Advantages
When you consult a neurosurgeon, you can expect:








