Arnold-Chiari malformation
Arnold-Chiari malformation is a rare congenital malformation that affects the development of the brain and spinal cord. It is characterized by displacement of the lower part of the brain – the cerebellum and cerebellum, with an asymmetrical arrangement of the cerebrum, posterior fossa and the sigmoid curve of the spinal cord. Because this complex anomaly can lead to serious health problems, decompression surgery is often necessary.
Decompression surgery for Arnold-Chiari malformation aims to relieve compression of nerve structures and provide better blood supply to the affected areas of the brain. The procedure involves removing part of the skull bone to reduce pressure on the posterior fossa and cistern of Lusca to improve blood circulation.
Diagnosis and preparation: our way to the operating room
Before I make a decision about surgical intervention, each patient undergoes a comprehensive examination.
- Clinical examination. We study the patient’s complaints in detail: the nature and localization of the headache, the presence of numbness or weakness in the limbs, coordination problems, which may indicate damage to the cerebellum.
- Neuroimaging. The basis of diagnosis is magnetic resonance imaging (MRI) . This is our main tool, allowing us to obtain an accurate image of cerebellar displacement, assess the degree of brainstem compression, and detect the presence of syringomyelia.
- Additional tests: Depending on your symptoms, we may order electromyography (EMG) to assess nerve damage or other functional tests.
Based on the data obtained, we develop an individual surgical plan, as each anomaly has its own unique characteristics.
Preparation for decompression surgery includes conducting a detailed medical examination of the patient, including:
- radiography,
- computed tomography (CT)
- magnetic resonance imaging (MRI).
This helps doctors get an accurate picture of the condition of Arnold-Chiari malformation and make an informed decision about the best treatment plan.
Decompression surgery: stages of intervention
The operation is usually performed under general anesthesia. Although the procedure itself may take several hours, the possible outcome is symptom relief and improved quality of life for the patient. However, as with any surgical procedure, there are risks and complications, so continued observation and monitoring of the patient’s condition is necessary.
I always explain every step to patients.
- Access formation. A small incision is made at the back of the head.
- Decompression. We remove part of the occipital bone (at the level where the cerebellum is displaced) and the arches of the first, and sometimes the second, cervical vertebrae. This creates additional space and relieves pressure on the neural structures.
- Duraplasty. This is followed by an intraoperative ultrasound examination. If the created space is not enough, I perform a duraplasty. This means that we cut the membrane and sew in a special “patch”, which can be made from the patient’s own tissues (aponeurosis, pericranium) or from biocompatible artificial materials. This procedure significantly increases the volume of the posterior cranial fossa, which is key to restoring normal cerebrospinal fluid circulation.
Postoperative period and rehabilitation
After decompression surgery, patients may need a period of rehabilitation to recover. This includes physical therapy and regular monitoring by medical staff. Depending on the individual patient’s condition, additional drug therapy or other treatments may be prescribed to further control symptoms.
The next stage is the patient’s recovery.
- Hospital stay. The patient remains under our supervision for several days. We monitor their condition, provide pain relief, and prevent possible complications such as infection or cerebrospinal fluid (CSF) leakage.
- Rehabilitation. After discharge, the rehabilitation period is individual. Most symptoms, such as headaches, usually disappear quite quickly. I recommend that patients do moderate physical therapy and avoid excessive exertion.
- Dynamic follow-up. We stay in touch with the patient. During the first year after surgery, we perform follow-up MRIs to evaluate the results and make sure that the cerebrospinal fluid is circulating properly and the syrinx is decreasing in size.
Overall, decompression surgery for Arnold-Chiari malformation is a complex procedure that can yield positive results for patients. However, before undergoing the procedure, patients should consult their doctor to discuss all aspects of the procedure, as well as potential risks and complications. The final decision to undergo decompression surgery should be made based on a careful examination and expert advice.
Operative decompression surgeries
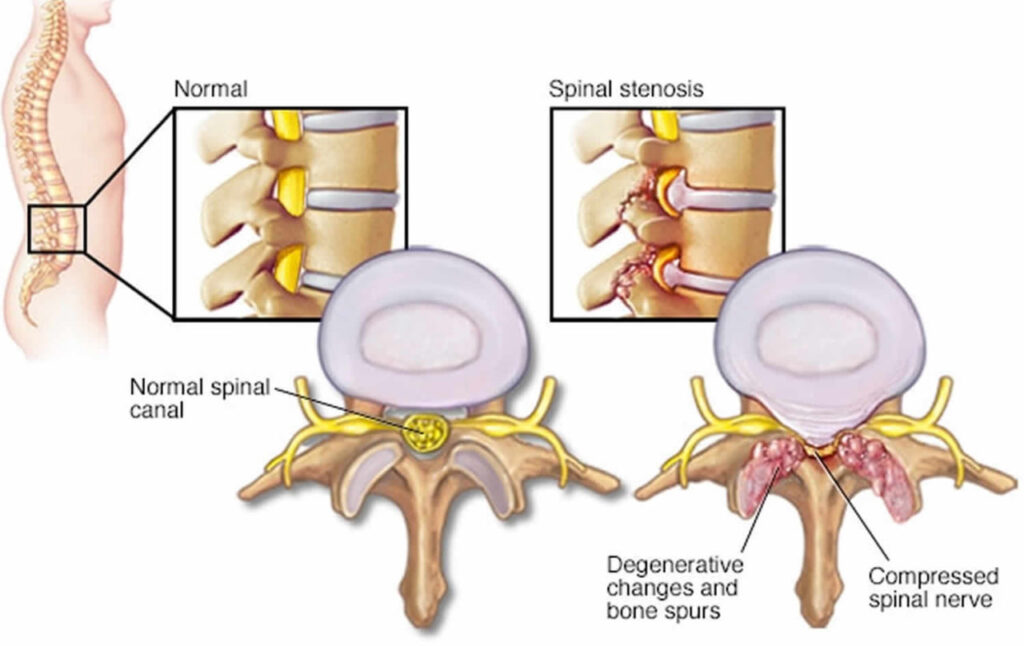
Surgical decompression surgeries are surgeries that are designed to relieve pressure on nerve tissue that is compressed or mechanically compressed. These surgeries can be performed on various parts of the body, including the spine, brain, nerves, and other organs. For example, spinal decompression surgery may be performed to relieve pressure on a disc that is compressing nerve tissue, which can cause pain and loss of function. The surgery may be performed open or minimally invasive. During surgery, the doctor may remove excess tissue that is compressing the nerve tissue or widen the space to relieve pressure on the nerve.
In some cases, your doctor may implant a device or make other adjustments to relieve pressure on the nerve. Decompression surgery can be an effective treatment for pain and other symptoms associated with nerve compression. However, like any surgery, it is not without risks and complications, such as bleeding, infection, and others. The decision to have surgery should be made after evaluating all the possible risks and benefits for each specific case.
The essence of the operation is to remove part of the occipital bone and the arch of the first, sometimes the second cervical vertebra. After that, an intraoperative ultrasound examination is performed to determine the created spaces for the circulation of cerebrospinal fluid. If these spaces are not enough, dura plasty is performed. The dura is cut and a “patch” is sewn in to increase the volume of the posterior cranial fossa. The role of the “patch” can be performed by both the patient’s own tissues (aponeurosis, bone) and artificial special prosthetic tissues.
Great, I’ll add a list of sources that meet the requirements of a popular science article. To make the article look more credible, you can add links to reputable medical resources and scientific publications that confirm the information.
Here is a list of sources that can be included at the end of the article, formatted in a bibliography style. I selected them based on a request, considering that this should not be a purely academic article, but rather an informative article for a wide audience.
Sources of information
- Chiari malformation: Symptoms and causes. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/chiari-malformation/symptoms-causes/syc-20354010
- Arnold-Chiari Malformation. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK431076/
- Surgical Treatment of Chiari I Malformation: Simplified Technique and Clinical Results. Journal of Neurosurgery. https://pmc.ncbi.nlm.nih.gov/articles/PMC1131847/
- Chiari Malformation and Syringomyelia: Diagnosis and Treatment. National Institute of Neurological Disorders and Stroke (NINDS). https://www.ninds.nih.gov/health-information/disorders/chiari-malformations
- Chiari malformation: Diagnosis and treatment. The National Health Service (NHS).
Стаття написана: 22.01.2026
Стаття перевірена медичним спеціалістом: 23.01.2026
Popular destinations:
Advantages
When you consult a neurosurgeon, you can expect: