The problem of syndromes in medicine
The problem of pain syndromes occupies a significant place in modern medicine, despite the large arsenal of surgical and conservative medical means of pain relief.
Very often, pain can be the only reason that forces a person to seek medical help, and, as a rule, our patients, due to their “mental characteristics”, suffer “until the last” and seek medical attention in the last stages of the disease.
Modern studies show that almost half of the country’s working-age population suffers from chronic pain, that is, pain that lasts for more than 6 months and often haunts a person for many years.
Pain syndromes can occur in patients after neurosurgical interventions. This pain can be due to various causes, including damage to nerve tissue, inflammation, infection, or stimulation of nerve structures.
The most common pain syndromes associated with neurosurgery are:
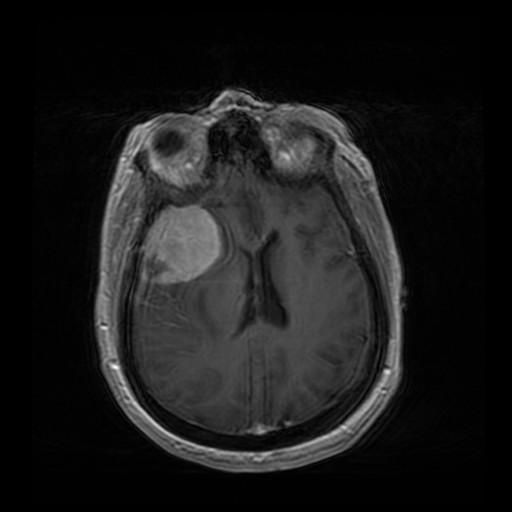
- Headache : After some neurosurgical procedures, such as brain tumor removal , patients may experience headaches. This may be due to damage to brain tissue or effects on the nervous system during the procedure.
- Trigeminal neuralgia. This is a chronic pain condition that results from damage to the trigeminal nerve in the face. This may be due to tumor removal, trauma, infection, or other causes.
- Back pain: Back pain can occur after neurosurgical procedures, especially spinal surgeries. This may be due to damage to the spinal cord or nerve roots that exit from it.
- Post-stroke pain syndrome. After a stroke, patients may experience pain in their body or limbs. This may be due to damage to nerve tissue as a result of the stroke.
Various methods can be used to treat pain syndromes in neurosurgery, including pharmacological drugs and physical therapy.
Vertebrogenic syndromes
Most often, neurosurgeons have to deal with pain caused by diseases of the spinal column – so-called vertebrogenic pain syndromes.
It is believed that by the age of 50, about 80% of men and up to 60% of women suffer from spinal diseases, and every second person among the adult population experiences vertebrogenic pain syndromes during their lifetime.
Most often, vertebrogenic pain syndromes are a consequence of spinal osteochondrosis – a disease that affects the intervertebral discs, with secondary involvement of “neighboring” anatomical formations in the process.
In cases of herniated intervertebral discs with compression of the structures of the spinal canal (most often the spinal roots), there is a fairly intense back pain that radiates into the leg.
As a rule, the pain is provoked by the vertical position of the body and active movements in the spine, with numbness and weakness in the leg, and may also be accompanied by dysfunction of the pelvic organs.
Types of spinal pathologies
Similar symptoms are observed in such spinal pathologies as narrowing (stenosis) of the spinal canal and spondylolisthesis (persistent displacement of the vertebrae relative to each other), instability of the spinal column.
With pathology of the intervertebral joints, the so-called “facet syndrome”, pain occurs or intensifies:
- when bending the body in different directions, weak, but sometimes radiates to the legs and usually not below the knee, worsens at night,
- as well as with monotonous postures, often occurs during sedentary work;
This pain is relieved by resuming active, habitual movements, “unloading” the spine.
Morning “stiffness” of the spine is also characteristic. Facet syndrome is not accompanied by sensory, motor, or pelvic disorders.
Disease
Chronic back pain can also be caused by diseases such as:
- consequences of spine and spinal cord injuries ,
- scoliosis (curvature of the spine),
- tumors of the spine and spinal cord.
Headache
Headache is also one of the most common and socially significant pain syndromes. In neurosurgical diseases , severe headache is usually found:
- in patients with traumatic brain injury and its consequences,
- with brain tumors ,
- with cerebral vascular pathology (aneurysms and arteriovenous malformations, which are complicated by the development of strokes),
- and also with hydrocephalus – excessive accumulation of fluid (CSF) in the ventricles of the brain, which has a different nature.
Clinic
Sometimes a headache can be caused by the above-mentioned cervical osteochondrosis. Most often, headaches in neurosurgical patients are caused by increased intracranial pressure and have typical features:
- “bursts”,
- diffuse nature of pain,
- its greatest intensity in the second half of the night and in the morning,
- the pain is accompanied by a feeling of pressure on the eyes from the inside,
- as well as the onset of sudden nausea and vomiting.
It should be noted that the most pronounced and prolonged pain syndrome is that in which the structures of the peripheral nervous system are involved in the pathological process , i.e., sensitive nodes, spinal roots, nerve trunks, etc.
Trigeminal neuralgia
Trigeminal neuralgia is a chronic condition characterized by repeated attacks of intense, shooting pain in the:
- in the frontal area,
- eyes,
- cheeks,
- jaw on one side of the face.
Pain attacks are provoked by irritation of the so-called “trigger” zones – small areas on the face, when irritated, a typical pain sensation occurs. Attacks of unbearable pain force patients to stop active activities, neglect personal hygiene, and the pain can lead a person to depression.
Shingles
Herpetic intervertebral neuralgia (also known as shingles) is a disease caused by the herpes virus and is usually triggered by hypothermia. Inflammation develops in sensitive nodes, which spreads to the nerves and roots.
The disease begins with general malaise, fever, and intense piercing pain in the intervertebral spaces, which worsens with movement.
After a few days, painful blisters filled with clear fluid appear at the site of the pain, which later turn into crusts. The process can become chronic and turn into the so-called postherpetic neuropathy with relapses of debilitating pain.
Upper extremity nerve involvement
Another pathology that often causes chronic pain is nerve impingement in the upper extremities, namely traumatic injuries and non-traumatic nerve entrapment.
Of particular note are carpal tunnel syndromes and ulnar nerve tunnel syndromes — non-traumatic entrapments, the so-called “tunnel syndromes.”
Complaints
With carpal tunnel syndrome, patients complain of:
- for numbness of the fingers (except the little finger),
- weakness in the hand and stiffness in the fingers (it is difficult to hold things in the hand),
- pain in the hand, which most often occurs at night and “radiates” to the forearm,
- as well as the gradual “drying” of the brush.
Manifestations
Cubital tunnel syndrome manifests itself:
- numbness in the little finger,
- ring finger,
- Pain in the elbow area (especially when moving the elbow joint), which worsens in cold weather.
Weakness and atrophy of small muscles also appear (a “hollow” is formed between the thumb and index finger), and the ability to bring the thumb to the hand is impaired.
Tunnel syndromes
The above-described “tunnel” syndromes lead to impaired function of the upper limb.
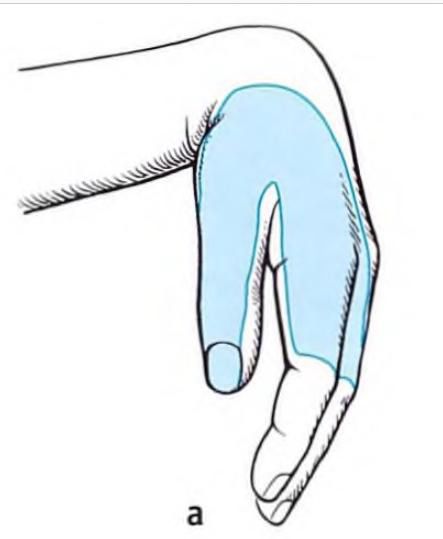
(dangling hand, radial nerve impingement)
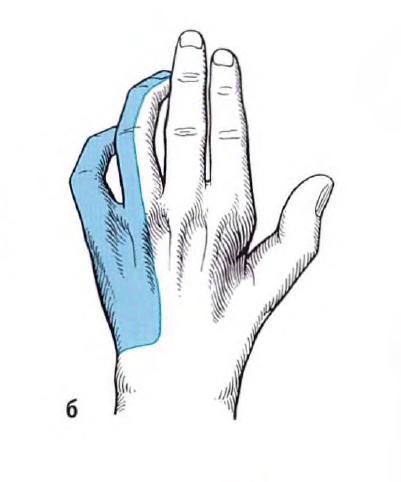
(clawed paw, ulnar nerve impingement)

(obstetrician’s hand, median nerve impingement)

(monkey hand, combined median and ulnar nerve impingement)
This, in turn, reduces both working capacity and the quality of life itself – a person, in essence, becomes “one-handed”, and if the impression is bilateral, completely “armless”.
However, we can say that the situation with the treatment of pain syndromes can still be viewed optimistically. The hospital actively employs a neurosurgeon with more than 20 years of experience, which employs highly qualified specialists.
Special modern equipment combined with medical skills and new technologies allow for the successful treatment of all of the above diseases at the level of world standards.
Стаття написана: 22.01.2026
Стаття перевірена медичним спеціалістом: 23.01.2026
Popular destinations:
Advantages
When you consult a neurosurgeon, you can expect: